In the world of medicine, some cases present diagnostic challenges that push even the most experienced clinicians to their limits. Today, we explore a gripping medical mystery, where methodical reasoning and attention to detail unveil the perfect diagnosis.
🩺 Case Presentation: The Puzzle Begins
A 45-year-old man arrives at the emergency department with persistent fatigue, intermittent fever, and unintentional weight loss over the past three months. He mentions occasional night sweats and a dry cough that worsens over time. Despite visiting multiple clinics, no clear diagnosis has been established.
Vitals:
Temperature: 38.3°C (100.9°F)
Heart rate: 98 bpm
Blood pressure: 128/82 mmHg
Respiratory rate: 20 breaths/min
Oxygen saturation: 96% on room air
📚 Step 1: History-Taking – Gathering Clues
The diagnostic journey begins with a thorough history, which holds vital clues.
-
Travel History: The patient recently traveled to Southeast Asia.
-
Social History: No smoking or alcohol use, but he volunteers at a local shelter.
-
Occupational History: Works in a factory with exposure to industrial chemicals.
Red Flags:
-
Persistent fever with weight loss suggests a chronic inflammatory or infectious process.
-
Recent travel raises suspicion for endemic infections.
-
His volunteering work hints at possible exposure to communicable diseases.
🩸 Step 2: Physical Examination – Detecting Subtle Signs
On examination:
-
General Appearance: Mild pallor, no jaundice, and no lymphadenopathy.
-
Chest Examination: Bilateral coarse crackles in the lower lung fields.
-
Abdomen: Mild splenomegaly without tenderness.
-
Neurological Examination: No focal deficits.
A high index of suspicion is raised for infectious, inflammatory, or hematologic causes.
🔬 Step 3: Initial Investigations – Narrowing Down Possibilities
Routine labs provide some answers:
-
CBC: Mild anemia (Hb 10.5 g/dL), leukocytosis with neutrophilia.
-
ESR/CRP: Elevated (suggesting inflammation).
-
Liver Function Tests: Mildly elevated transaminases.
-
Chest X-ray: Bilateral reticulonodular opacities.
🔹 Provisional Diagnosis: Tuberculosis (TB) or fungal infection is high on the differential due to the subacute presentation, chronic cough, and travel history.
🧠 Step 4: Advanced Diagnostics – Digging Deeper
To refine the diagnosis:
-
CT Chest: Bilateral nodular infiltrates with cavitation.
-
Bronchoscopy with BAL: Negative for acid-fast bacilli (AFB).
-
Blood Cultures: No bacterial growth after 48 hours.
-
Serology: Positive IgM for Histoplasma capsulatum.
💡 Diagnostic Clue: A positive Histoplasma test suggests histoplasmosis, a fungal infection endemic to certain regions, including Southeast Asia.
🕵️ Step 5: Piecing It Together – Solving the Mystery
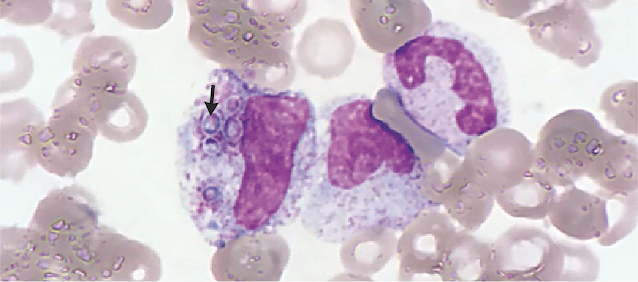
With a strong suspicion of disseminated histoplasmosis, a bone marrow biopsy is performed, revealing intracellular yeast forms consistent with Histoplasma capsulatum.
✅ Final Diagnosis: Disseminated Histoplasmosis
The diagnosis explains the patient’s chronic fever, weight loss, and pulmonary findings. Immunocompromised conditions were ruled out, reinforcing that exposure to an endemic area was the primary risk factor.
💊 Step 6: Initiating Treatment – Turning the Tide
The patient is promptly started on:
Liposomal Amphotericin B for induction therapy.
Transitioned to Itraconazole for long-term maintenance.
Clinical improvement is noted within weeks, with resolution of fever and improved respiratory function.
📖 Key Lessons from the Case
-
Thorough History is Key: Subtle details like travel and volunteering uncovered critical diagnostic clues.
-
Multimodal Investigation: Imaging, microbiology, and histopathology confirmed the diagnosis.
-
Consider Endemic Infections: Especially in cases with travel to high-risk regions.
For medical students and clinicians, solving a high-stakes diagnostic puzzle requires patience, critical thinking, and a systematic approach. Access detailed diagnostic guides and case studies on MedNotes to refine your clinical reasoning skills.
🔍 Conclusion: The Art of Diagnosis
In challenging cases like this, arriving at the correct diagnosis is like piecing together a complex puzzle. With a step-by-step approach and the right tools, the perfect diagnosis is always within reach.
Explore more clinical case breakdowns and diagnostic tips on MedNotes.